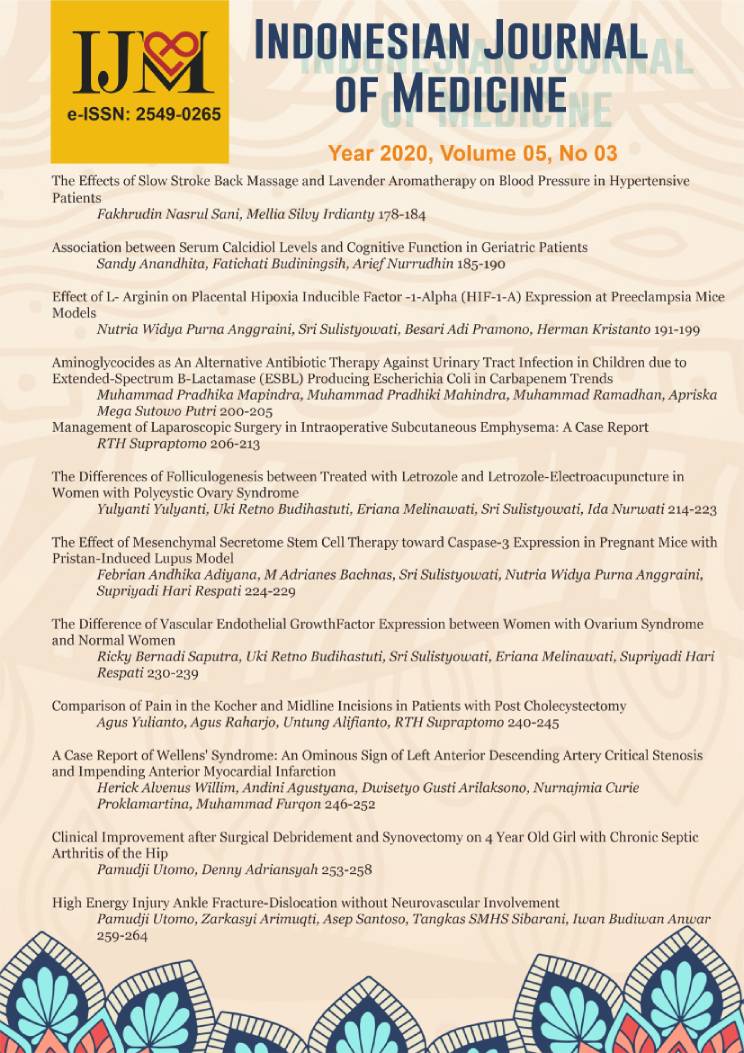
The Difference of Endometrial Vascular Endothelial Growth Factor (VEGF) Expression between Polycystic Ovarian Syndrome (PCOS) and Normal Women
DOI:
https://doi.org/10.26911/theijmed.2020.5.3.296Abstract
Background: Polycystic Ovarian Syndrome (PCOS) is an endocrine disorder in women characterized by increased levels of androgens, ovulatory dysfunction, and Polycystic Ovarian Morphology (PCOM), as well as a combination of classic clinical features. Women with PCOS experience changes in the endometrium and endometrial receptivity markers such as VEGF (Vascular Endothelial Growth Factor). VEGF increases the permeability and dilation of endometrial blood vessels which play an important role in implantation. This study aimed to analyze the difference of VEGF expression between women with PCOS and normal women.
Subjects and Method: This study was a case-control study design conducted at the polyclinic of the Department of Obstetrics and Gynecology, Dr. Moewardi Hospital, Surakarta, Central Java, in July 2020. There were 30 infertile women with PCOS (diagnosis based on Rotterdam criteria, consensus 2003) and 30 women without PCOS as the sample of this study. The dependent variable was VEGF expression. The independent variables were age, BMI, family history with PCOS, menarche, occupation, and education. VEGF expression was obtained from an endometrial biopsy on days 19-24 of periods. The differences in VEGF expression (in %) were analyzed by the Mann-Whitney test. VEGF determinants were analyzed by a multiple linear regression.
Results: The mean of VEGF expression in women with PCOS (Mean=64.33; SD=44.43) was higher than in women without PCOS (Mean= 7.90; SD=8.73) and the result was statistically significant (p<0.001). PCOS (b=42.09; 95%CI=64.26 to -19.93; p<0.001) and obese (b=38.63; 95%CI=-63.44 to -13.82; p=0.003) increased VEGF expression.
Conclusion: VEGF expression in the endometrium of women with PCOS is higher than normal women.
Keywords: VEGF, endometrium, Polycystic Ovarian Syndrome
Correspondence: Ricky Bernadi Saputra. Department of Obstetrics and Gynecology, Faculty of Medicine, Universitas Sebelas Maret/ Dr. Moewardi Hospital, Surakarta, Indonesia. Telp: 081221161933 Email: rickysaputradr@gmail.com
Indonesian Journal of Medicine (2020), 05(03): 230-239
https://doi.org/10.26911/theijmed.2020.05.03.08
References
Almawi WY, Gammoh E, Malalla ZH, Al-Madhi SA (2016). Analysis of VEGFA Variants and Changes in VEGF Levels Underscores the Contribution of VEGF to Polycystic Ovary Syndrome. PLoS ONE 11(11): e0165636. https://doi.org/10.1371/journal.pone.0165636.
Diamanti-Kandarakis E, Piperi C, Korkolopoulou P, et al. (2007). Accumulation of dietary glycotoxins in the reproductive system of normal female rats. J Mol Med (Berl). 2007;85(12):1413-14-20. doi:10.1007/s00109-007-0246-6.
Harada M, Peegel H, Menon KM (2010). Expression of vascular endothelial growth factor A during ligand-induced down-regulation of luteinizing hormone receptor in the ovary. Mol Cell Endocrinol. 328(1-2): 28–33. https://dx.doi.org/10.1016%2Fj.mce.2010.06.015.
Kandaraki E, Chatzigeorgiou A, Piperi C, Palioura E, Palimeri S, Korkolopoulou P, Koutsilieris M, Papavassiliou AG (2012). Reduced ovarian glyoxalase-I activity by dietary glycotoxins and and rogen excess: a causative link to polycystic ovarian syndrome. Mol Med: 18(1): 1183-1189. ttps://dx.doi.org/10.2119%2Fmolmed.2012.00293.
Lai TH, Vlahos N, Shih IeM, Zhao Y (2015). Expression Patterns of VEGF and Flk-1 in Human Endometrium during the Menstrual Cycle. J Reprod Infertil. 16(1): 3-9. https://www.ncbi.nlm.nih.gov/pubmed/25717429.
Legro RS (2012). Obesity and PCOS: Implications for diagnosis and treatment. Semin Reprod Med, 30(6): 496-506. doi: 10.1055/s-0032-1328878.
Mukherjee S, Maitra A (2010). Molecular genetic factors contributing to insulin resistance in polycystic ovary syndrome. Indian J Med Res. 131:743-760.
Peitsidis P, Agrawal R (2010). Role of vascular endothelial growth factor in women with PCO and PCOS: A systematic review. Reproductive BioMedicine Online (20): 444– 452. https://doi.org/10.1016/j.rbmo.2010.01.007.
Repaci A, Gambineri A, Pasquali R (2011). The role of low-grade inflammation in the polycystic ovary syndrome. Mol Cell Endocrinol, 335(1): 30–41. https://doi.org/10.1016/j.mce.2010.08.002.
Ring M (2017). Polycystic ovarian syndrome, menopause, and osteoporosis. Prim Care Clin Office Pract. (44): 377–398. https://doi.org/10.1016/j.pop.2017.0-2.012.
Rojas J, Chávez M, Olivar L, Rojas M, Morillo J, Mejías J, Calvo M, Bermúdez V (2014). Polycystic ovary syndrome, insulin resistance, and obesity: navigating the patho-physiologic labyrinth. Int J Reprod Med. 719050. doi:10.1155/20-14/719050.
Sachdeva G, Gainder S, Suri V, Sachdeva N, Chopra S (2019). Obese and non-obese polycystic ovarian syndrome: comparison of clinical, metabolic, hormonal parameters, and their differential response to clomiphene. Indian J Endocrinol Metab, 23(2): 257–262. doi: 10.41-03/ijem.IJEM_637_18.
Schneider D, Gonzalez JR, Yamamoto M, Yang J, Lo JC (2019). The Association of Polycystic Ovary Syndrome and Gestational Hypertensive Disorders in a Diverse Community-Based Cohort. J Pregnancy, 9847057: 1-6. https://dx.doi.org/10.1155%2F2019%2F9847057
Scotti L, Parborell F, Irusta G, De Zuñiga I, Bisioli C, Pettorossi H, Tesone M, Abramovich D (2014). Platelet-derived growth factor BB and DD and angio-poietin1 are altered in follicular fluid from polycystic ovary syndrome patients. Mol Reprod Dev. 81(8): 748-756. https://doi.org/10.1002/mrd.22343.
Sumapraja K, Pangastuti N (2011). Profile of Policystic Ovarian Syndrome Patients in Dr. CiptoMangunkusumo General Hospital Jakarta March 2009 March 2010. Indonesian Journal of Obstetrics and Gynecology, 35(1).
Tahergorabi Z, Salmani F, Jonaidabad SH, et al. (2019). Association of serum levels of vascular endothelial growth factor and thrombospondin-1 to body mass index in polycystic ovary syndrome: a case-control study. Obstet Gynecol Sci. 62(6): 420-428. doi: 10.5468/ogs.2019.62.6.420.
Yoshii N, Hamatani T, Inagaki N, Hosaka T, Inoue O, Yamada M, Machiya R, Yoshimura Y, Odawara Y (2013). Successful implantation after reducing matrix metalloproteinase activity in the uterine cavity. Reprod Biol Endocrinol, 11:37. https://dx.doi.org/10.1186%2F1477-7827-11-37.
Zhao DM, Shan YH, Li FH, Jiang L, Qu QL (2019). Correlation between endometrial receptivity with expressions of IL-1 and VEGF in rats with polycystic ovary syndrome. Eur Rev Med Pharmacol Sci, 23(13): 5575-5580. doi: 10.26355/eur-rev_201907_18291.