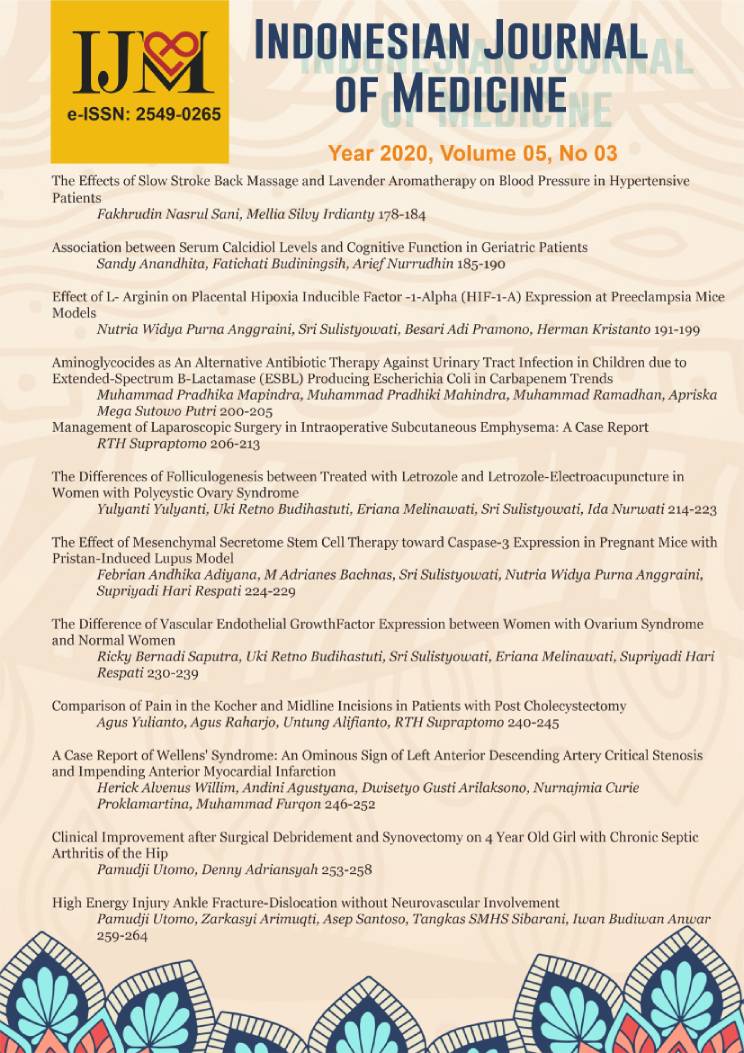
Effect of L- Arginin on Placental Hipoxia Inducible Factor -1-Alpha (HIF-1-A) Expression at Preeclampsia Mice Models
DOI:
https://doi.org/10.26911/theijmed.2020.5.3.290Abstract
Background: Placental hypoxia is one of the theories that cause preeclampsia. In placental hypoxia of preeclampsia, there is an increase of Hipoxia Inducible Factor 1 Alpha (HIF-1-A) expression as a response to hypoxia. L-Arginine administration through the L-Arginine-Nitric Oxide pathway is expected to improve placental hypoxia. This study aimed to examine the effect of L- Arginin on placental HIF-1-A expression at preeclampsia mice models.
Subjects and Method: Experimental study with parallel group post-test only design. The study was carried out at the Veterinary Medicine Faculty of Airlangga University. Thirty six preeclampsia mice models were made with intravenous injection 10ng anti-Qa-2 on day 1-4 of pregnancy. They were divided into 2 groups: (1)18 mice without treatment (control) and (2) 18 mice were given L-Arginin 200 mg/kgBW/day on day 7-15 of pregnancy. They were terminated on day 16 then immunohistochemistry examination of HIF-1-A expression was done on the placental samples. The dependent variable was placental Hipoxia Inducible Factor-1-Alpha (HIF-1-A) expression. The independent variables were L-Arginin administration. HIF-1-A expression was measured by H-Score method. The data were analyzed by t-test.
Results: The mean of placental HIF-1-A expressions of treatment group was lower (Mean= 7.98; SD=9.35) than control group (Mean=41.95; SD= 32.20), and it was statistically significant (p <0.001).
Conclusion: L-Arginin reduces the Placental Hypoxia Inducible Factor Alpha (HIF-1-A) expression on preeclampsia mice model.
Keywords: L-Arginine, HIF-1-A, Preeclampsia
Correspondence: Nutria Widya Purna Anggraini. Department of Obstetrics and Gynecology, Faculty of Medicine Universitas Sebelas Maret/ Dr. Moewardi General Hospital Surakarta. Jl Kolonel Sutarto 132, Surakarta, Central Java, Indonesia. Email: nutria_dr@staff.uns.ac.id. Mobile: 08122651819.
Indonesian Journal of Medicine (2020), 05(03): 191-199
https://doi.org/10.26911/theijmed.2020.05.03.03
References
Al-Bayati MA, Ahmad MA, Khamas W (2014). The potential effect of l-arginine mice placenta. Adv Pharmacoepidemiol Drug Saf, 3(2): 1-9. https://doi.org/0.4172/2167-1052.1000150.
Asif A and Wenda R (2015). Unraveling the theories of pre-eclampsia: are the protective pathways the new paradigm?. Br J Pharmacol, 172(6): 1574–86.
Burke S and Karumanchi (2013). A Spiral artery remodeling in preeclampsia revisited. Hypertension,(62) :1013-4.
Cheryl LML (2015). Female reproductive tract. In : A practical Guide Hystology of the Mouse. 6th ed. Milton (Australia): John Wiley 7 Sons, p.88-97.
Facchinetti F, Farulla A. (2017)Dietary suplements and drugs for preeclampsia prophylaxis. Journal of Women’s Cardiovascular Health. (7): 59 https://doi.org/10.1016/j.preghy.2016.10.014.
Gao K, Jiang Z, Lin Y, Zheng C, Zhou G, Chen F, Wu G (2011). Dietary l-arginine supplementation enhances placental growth and reproductive performance in sows. Amino Acids, 42(6), 2207–2214. https://doi.org/10.1007/s00726-011-0960-9.
Grafka A, Lopucki M, Karwasik-Kajszczarek K, Stasiak-Kosarzycka M, Miturski A, Dzida G (2016). Study of the role l-arginine in the diagnosis of pregnancy induced hypertension Arterial Hypertens, 20 (3): 113-8.
Himpunan Kedokteran Fetomaternal (2017). Pedoman nasional pelayanan kedokteran tata laksana komplikasi kehamilan. Jakarta: Kementerian Kesehatan Republik Indonesia,hal. 23-48.
Kooffreh ME, Ekott M, Ekpoudom DO (2014). The prevalence of preeclampsia among pregnant women in the university of calabar teaching hospital, calabar. Saudi J Health Sci, (3):133-6. https://doi.org/10.4103/2278-0521.142317.
Korkes HA, De Oliveira L, Sass N, Salahuddin S, Karumanchi SA, Rajakumar A (2017). Relationship between hypoxia and downstream pathogenic pathways in preeclampsia. Hypertension in Pregnancy, 36(2), 145–150. https://doi.org/10.1080/10641955.2016.1259627.
Ibrahim NA, Khaled DM (2014). Histological and immunohistochemical study on human placental tissue in normal pregnancy and preeclampsia. Nat Cell Biol, 2(6): 72-80. https://doi.org/10.11648/j.cb.20140206.13.
Lassala A, Bazer FW, Cudd TA, Datta S, Keisler DH, Satterfield MC, Spencer TE, et al (2011). Parenteral adminis-tration of l-arginine enhances fetal survival and growth in sheep carrying multiple fetuses. J Nutr, 141(5): 849–55. https://doi.org/10.3945/jn.111.13-8172.
Lyall F, Bellfort MA (2007). Preeclampsia: etiology and clinical practice. New York: Cambridge University Press.
Ohta H, Kaga M, Li H, Sakai H, Okamura K, Yaegashi N (2017). Potential new non-invasive therapy using artificial oxygen carriers for preeclampsia. J Funct Biomater. 8(3): 32. https://doiorg/10.3390/jfb8030032.
Patel J, Landers K, Mortimer RH, Ricard K (2010). Regulation of hypoxia inducible factors (HIF) in hypoxia and normoxia during placental development. Placenta. 31(11): 951-7. https://doi.org/10.1016/j.placenta.2010.08.008.
Provincial Health Office of Central Java (2015). Profil kesehatan provinsi jawa tengah tahun 2015[internet]. Available from: https://www. Dinkesjatengprov.go.id/v2015/dokumen/profil2015/.
Robb KP, Cotechini T, Allaire C, Sperou A, Graham CH (2017). Inflammation-induced fetal growth restriction in rats is associated with increased placental HIF-1α accumulation. Plos One, 12-(4), e0175805. https://doi.org/10.1371/journal.pone.0175805.
Sánchez-Aranguren LC, Prada CE, Riaño-Medina CE, Lopez M (2014). Endo-thelial disfunction and preeclampsia: role of oxidative stress. Front Physiol. (5): 372. https://doi.org/10.3389%2Ffphys.2014.00372.
Tal R (2012). The role of hypoxia and hypoxia inducible factor 1 alpha in preeclampsia pathogenesis. Biol Reprod, 87(6): 1-8. https://doi.org/10.1095/biolreprod.112.102723.
Roberts JM, Hubel CA (2009). The two stage model of preeclampsia: variations on the theme. Placenta. (23): 32–7. https://doi.org/10.1016%2Fj.placenta.2008.11.009.
Roberts MD, Phyllis A (2013). Task force on hypertension in pregnancy. In: Hypertension in pregnancy. ACOG. (2): 1-11. Available from: https://www.acog.org/Clinical/Taskforce.
Semenza G (2011). Hypoxia inducible factor 1: ;Regulator of mitochondrial metabolism and mediator of ischemic pre-conditioning. Biochim Biophys Acta. 13(7): 1263-8.
Soetrisno S, Sulistyowati S, Wibowo AS (2017). L-arginine improves uterine spiral arterial wall thickness in mouse model of preeclampsia. Univ Med. 36 (2):131-7.
Supranto J (2010). Teknik sampling untuk survey dan eksperimen. Jakarta: PT. Rineka Cipta.
Verma S, Pillay P, Naicker T, Moodley J, Mackraj I (2018). Placental hypoxia inducible factor-1α CHOP immuno-histochemical expression relative to maternal circulatory syncytiotrophoblast micro-vesicles in preeclamptic and normotensive pregnancies.
Eur J Obstet Gynecol Reprod Biol. 220: 18-24. https://doi.org/10.1016/j.ejogrb.2017.11.004.
Wall TD, Grivell RM, Dekker GA, Hague W, Dodd JM (2014). The role of L-Arginin in the prevention and treatment of pre-eclampsia: a systematic review of randomised trials. J Hum Hypertens, 28(4): 230–5.
Wantania J, Bakri S, Pandelaki K, Chalid M (2013). Altered level of soluble fms like tyrosine kinase 1 (sFlt1) and hypoxia inducible factor 1alpha (HIF-1Alpha) in normotensive pregnancy and preeclampsia. Indones Biomed J. 5(2): 121-8. https://doi.org/10.18585/inabj.v5i2.61.
Woods AK, Hoffmann DS, Weydert CJ, Butler SD, Zhou Y, Sharma RV, Davisson RL (2011). Adenoviral delivery of vegf 121 early in pregnancy prevents spontaneous development of preeclampsia in bph/5 mice. Hypertension. 57(1): 94-102. https://doi.org/10.1161/hypertensionaha.110.160242.