Aminoglycocides as An Alternative Antibiotic Therapy Against Urinary Tract Infection in Children due to Extended-Spectrum Β-Lactamase (ESBL) Producing Escherichia Coli in Carbapenem Trends
DOI:
https://doi.org/10.26911/theijmed.2020.5.3.260Abstract
Background: Extended-spectrum β-lactamase (ESBL) is an enzyme produced by certain Escherichia coli and Klebsiella pneumoniae. ESBL can induce theantibiotic resistance for betalactam antibiotics such as penicillin, cephalosporin, etc. Frequent utilization of carbapenem may induce the risk for carbapenem resistant against ESBLs producing microorganisms. This stud aimed to communicate Aminoglycocides as an alternative antibiotic therapy against urinary tract infection in children.
Case Presentation: We present a case of 4 years child who was admitted to the state hospital of Madiun with main complaint of 10 days high fever accompanied by phimosis appearance. Laboratory results based on urine culture show the ESBL positive Escherichia coli.
Results: We have used aminoglycoside for treating the patient. Clinical presentation in this patient start showing an improved clinical response and negative bacteriuria in the second urine test after the aminoglycoside therapy.
Conclusion: Aminoglycosides such as gentamicin can be considered to be one of the best options for treating an ESBL infection beside carbapenem in order to reduce the carbapenem trend In clinical setting of the urinary tract infection caused by ESBL Eschericia coli.
Keywords: Aminoglycosides, Carbapenem, Extended-spectrum β-lactamase, Gentamicin, urinary tract infection
Correspondence: Muhammad Pradhika Mapindra. General Practitioner in State Hospital of Madiun, Easy Java. Email: mpradhika57@gmail.com.
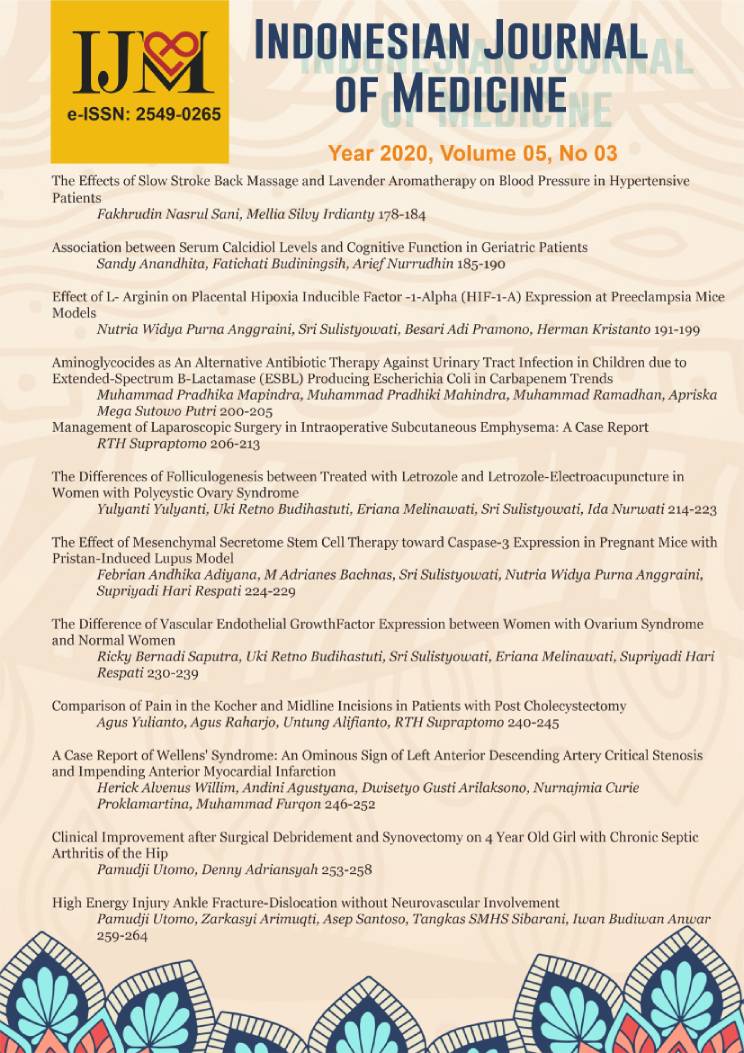
Indonesian Journal of Medicine (2020), 05(03): 200-205
https://doi.org/10.26911/theijmed.2020.05.03.04
References
Andrews JM (2001). Determination of minimum inhibitory concentrations. J Antimicrob, 48(S1): 5–16.
Bitsori M, Galanakis E (2019). Treatment of Urinary Tract Infections Caused by ESBL-producing Escherichia coli or Klebsiella pneumoniae. Pediatr Infect. Dis J. 38(12): e332–e335. doi: 10.1097/INF.0000000000002487.
Day MJ, Hopkins KL, Wareham DW, Toleman MA, Elviss N, Randall L, Cleary P, et al. (2019). Extended-spectrum β-lactamase-producing Escherichia coli in human-derived and food chain-derived samples from England, Wales, and Scotland: an epidemio-logical surveillance and typing study. Lancet Infect Dis. 19(12): 1325–1335. doi: 10.1016/S1473-3099(19)30273-7.
Kanematsu A (2016). Management of phimosis as a risk factor of urinary tract infection: An Asian perspective. Urol Sci. 27(4): 190–192. doi: 10.1016/j.-urols.2016.08.005.
Kumar D, Singh AK, Ali MR, Chander Y (2014). Antimicrobial susceptibility profile of extended Spectrum β-Lactamase (ESBL) producing Escherichia coli from various clinical samples. Infect Dis (Auckl). 7: 1-8. doi: 10.4137/idrt.s13820.
Paterson DL, Bonomo RA (2005). Clinical update extended spectrum beta-lactamases: A clinical update. Clin Micro-biol. 18(4): 657–686. doi: 10.1128/C-MR.18.4.657.
Puvabanditsin S, et al. (2019). Extended-spectrum beta-lactamase-producing Escherichia coli meningitis and cere-bral abscess in a neonate: Therapeutic Challenge. Case Reports Infec Dis. 1–5. doi: 10.1155/2019/6874192.
Ramlakhan S, Singh V, Stone J, Ramtahal A (2014). Clinical options for the treatment of urinary tract infections in children. Clin Med Insights: Pedia-trics. 8: 31–37. https://doi.org/10.41-37/CMPed.S8100.
Singh Grewal D, Macdessi J, Craig J (2005). Circumcision for the preven-tion of urinary tract infection in boys: A systematic review of randomised trials and observational studies. Arch Dis Child. 90(8): 853–858. doi: 10.-1136/adc.2004.049353.
Walker KJ, Lee YR, Klar AR (2018). Clinical outcomes of extended-spectrum beta-lactamase-producing enterobacteriaceae infections with susceptibilities among Levofloxacin, Cefepime, and Carbapenems. Can J Infect Dis Med Microbiol. doi: 10.1155/2018/3747521.
Zohar I, Schwartz O, Yossepowitch O, David SSB, Maor Y (2020). Aminoglycoside versus carbapenem or piperacillin/tazobactam treatment for bloodstream infections of urinary source caused by Gram-negative ESBL-producing Enterobacteriaceae. J Antimicrob Chemother. 75(2): 458–465. doi: 10.1093/jac/dkz457.